Step 1 in Improving Fertility: Regulating Hormonal Balance
Date: 02/28/2025
When women planning for pregnancy want to assess their fertility, one of the essential tests is the six – hormone assay for sex hormones. Although it is a simple blood test, it can potentially reveal the reasons why a woman has long failed to conceive naturally or has experienced repeated failures in in – vitro fertilization (IVF).
Today, TCC will guide you through understanding why we consider hormonal balance as the first step in enhancing fertility.
- The Relationship between Sex Hormones and Fertility
Hormones are chemical messengers in the human body, playing a crucial role in various aspects such as metabolism, growth, development, and reproduction.
The six – hormone assay for sex hormones, which is primarily related to fertility, includes follicle – stimulating hormone (FSH), luteinizing hormone (LH), estradiol (E2), progesterone (P), testosterone (T), and prolactin (PRL).
Among these six sex hormones, FSH, LH, E2, and P are most closely related to egg development and endometrial growth.
Group 1
Under normal circumstances, in the early stage of the menstrual cycle, the pituitary gland, which controls the endocrine system, will issue instructions to the ovaries through FSH and LH based on the condition of the eggs in the previous cycle. These instructions include promoting the growth of oocytes, stimulating follicles, the proliferation of granulosa cells, and ovulation.
FSH (Follicle – Stimulating Hormone): As its name implies, its main function is to promote follicle growth. The egg develops and grows within the follicle by accumulating nutrients.
LH (Luteinizing Hormone): Its main function is to promote the further maturation and release of eggs. Subsequently, the follicle transforms into a corpus luteum, preparing for the implantation of the fertilized egg.
Group 2
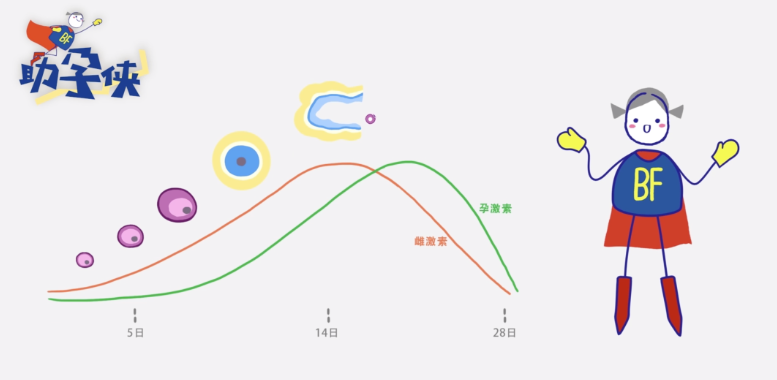
E2 is estradiol, and P is progesterone. The ovaries will convey this group of hormones to the pituitary gland, and then the pituitary gland adjusts its instructions according to the feedback.
E2 is secreted by the granulosa cells in the follicle, reflecting the progress of follicle development. Generally, the higher the E2 level, the larger the volume of the follicle. To a certain extent, it also indicates that the follicle is more mature, and the core egg can absorb more sufficient nutrients.
Progesterone (P) is a feedback after ovulation is completed. After the egg is released, the ruptured or emptied follicle will transform into a corpus luteum, secreting a large amount of P while secreting E2. The pituitary gland, upon receiving the reports of E2 and P, will gradually reduce FSH and LH, suspend ovarian ovulation, and adjust the uterine cavity state to welcome the arrival of the embryo. If no embryo arrives, the corpus luteum will begin to atrophy, and E2 and P will decline accordingly.
Normally, the changes of these hormones basically advance synchronously with the menstrual cycle, follicle development, and endometrial transformation, showing regular cyclic changes. Once imbalanced, it is likely to affect the growth rhythm of follicles and endometrial transformation, leading to a decrease in fertility. - The Impact of Hormonal Imbalance on Pregnancy Preparation
Elevated FSH
Causing Premature Follicle Growth
Generally, an FSH value higher than 10 in the early stage of the menstrual cycle means that the pituitary gland has issued a stronger instruction to make the follicles in the ovary grow as soon as possible. However, although the finally formed follicle may seem to be a mature follicle on the surface and can ovulate normally, in fact, its growth time is much shorter than that of a normal follicle. As a result, the egg inside does not store enough nutrients and energy, resulting in poor egg quality. This may lead to difficulties in fertilization or poor embryonic development potential.
Abnormal LH Affecting Ovulation
If the LH value is too high in the early stage of the menstrual cycle, especially when the LH/FSH ratio is greater than 2, it means that the pituitary gland has issued an instruction to promote follicle maturation and ovulation. But in fact, in the early stage of the menstrual cycle, the follicles are small in size, and such an instruction will cause small follicles to accumulate and develop slowly.
During the ovulation period, the LH level should reach at least 2.5 times the initial value to indicate that the eggs can mature and be discharged well. If it does not reach this level, it often means that the eggs are not mature enough and of poor quality. However, it is not the case that the higher the peak value, the better. One of the manifestations of polycystic ovary syndrome is an excessively high LH level, which indicates that the ovary has accumulated a large number of small follicles, the follicles grow and develop slowly, and the egg quality is not up to standard.
E2 Reflecting Follicle Growth and Promoting Endometrial Growth
There is a negative feedback relationship between E2 and FSH. On the other hand, E2 is also an essential hormone for endometrial growth.
If E2 is too high in the early stage of the menstrual cycle, the pituitary gland will think that the follicles have matured and will secrete LH in advance, making the ovary receive the information that it can ovulate. This may cause the eggs to be discharged prematurely before they are fully developed. However, if E2 is too low, the pituitary gland will judge that the follicles are not mature enough and will increase FSH secretion, repeating the situation of high FSH mentioned above, and the egg quality cannot be guaranteed.
P (Progesterone) Affecting Endometrial Transformation
Before ovulation, progesterone remains at a low level. With the occurrence of ovulation and the formation of the corpus luteum, more progesterone will be secreted. At this time, the endometrium begins to become soft, blood flow will increase accordingly, and the immune state of the uterine cavity will also change. If the corpus luteum function is low, it will cause a low P level, thus affecting the overall transformation of the endometrium and the implantation and development of the embryo.
Among the commonly seen hormonal imbalances in daily life, the imbalance of FSH and LH is the most common. For example, a high FSH level or insufficient LH secretion will affect follicle development and egg quality. In fact, the imbalance between E2 and P also occurs frequently. If E2 is too high and P is insufficient, it will lead to a decrease in endometrial receptivity and affect the implantation and development of the embryo. - How to Improve the Situation of Hormonal Imbalance
Identifying the Cause and Precise Intervention
The relationship between hormones is one of mutual promotion and influence. Metabolic abnormalities often lead to hormonal changes. For example, insulin resistance may lead to an increase in LH, and FSH may change significantly due to high stress. Therefore, it is necessary to analyze the report values to find the cause, identify the point of hormonal imbalance, and then carry out precise intervention.
Synchronizing Medication and Lifestyle Interventions
If necessary, medication intervention can also be adopted. For example, progesterone can increase the progesterone level, thereby promoting endometrial improvement for better embryo implantation. Therefore, when the corpus luteum function is insufficient, progesterone is often used for regulation. Appropriate use of estrogen in the follicular phase can help reduce FSH, control the follicle growth rhythm, and appropriately extend the development time.
In addition to medication intervention, lifestyle interventions can also be carried out simultaneously to adjust hormonal imbalances caused by metabolic and immune abnormalities. Only by treating both the symptoms and the root causes can we truly promote the normal development of follicles and the improvement of endometrial receptivity, thereby increasing the pregnancy success rate.
相关推荐
- 5 Key Daily Habits to Improve IVF Success in 2025
- 35+ Women’s Guide to Scientific Preparation for Pregnancy: Medical Strategies and Health Management for Fertility at Advanced Ages
- Follicular phase determines the golden window for fertility success
- Second Generation IVF Technology (ICSI Technology) on Offspring Health Implications
- Egg Maturity Mystery: Why IVF Retrieves Many Eggs but Few Embryos?
Search within the site
Surrogacy News
Hot Tags.
Georgia Surrogacy Services,Legal IVF Hospital,Global Fertility Agency