New breakthrough in the treatment of polycystic ovary syndrome: targeting TNF-α inhibitors to enhance fertility success rate
I. TNF-α: a core driver of inflammation in polycystic ovary syndrome (PCOS)
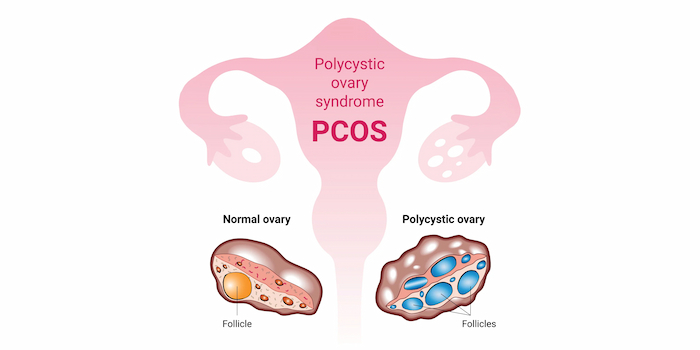
Polycystic ovary syndrome (PCOS) is a complex endocrine-metabolic disease characterized by hyperandrogenemia, insulin resistance, and ovulatory disorders. Recent studies have found that chronic inflammatory state is the core pathological mechanism of PCOS, and tumor necrosis factor-α (TNF-α), as a key inflammatory mediator, crosstalks pathological processes such as oxidative stress, insulin resistance, obesity and hormonal imbalance.
- The vicious cycle of TNF-α and oxidative stress
Oxidative-antioxidant imbalance: reactive oxygen species (ROS) levels are significantly elevated in PCOS patients, and TNF-α further stimulates ROS production by activating the NF-κB pathway, creating a self-reinforcing inflammatory-oxidative stress cycle.
Ovarian cell damage: Excessive ROS directly impaired the mitochondrial function of follicular granulosa cells, leading to follicular developmental stagnation and ovulation disorders.
- TNF-α exacerbates insulin resistance (IR)
Receptor dysfunction: TNF-α inhibits insulin signaling by phosphorylating insulin receptor substrate-1 (IRS-1) and reduces the activity of glucose transporter protein GLUT-4, leading to abnormal glucose metabolism.
Visceral fat accumulation: insulin resistance promotes fat accumulation in the abdomen, and visceral adipose tissue releases more TNF-α, forming a positive feedback of “metabolism-inflammation.
- TNF-α regulates hyperandrogenemia
Enhancement of androgen synthesis: TNF-α activates ovarian CYP17A1 enzyme, which directly promotes testosterone production, and inhibits aromatase activity, which hinders the conversion of testosterone to estrogen49.
Sex hormone-binding globulin (SHBG) inhibition: increases the bioactivity of free testosterone by decreasing hepatic SHBG levels.
II. Anti-TNF-α therapy: from animal model to clinical validation
- Breakthrough findings from animal experiments
DHEA-induced PCOS model: In female rats, the use of dehydroepiandrosterone (DHEA) induced PCOS-like symptoms manifested by ovarian polycysticity, hormonal imbalance and metabolic disorders.
Etanercept (Etanercept) intervention effect: After 35 days of combined DHEA and TNF-α inhibitor Etanercept treatment, rats showed restoration of ovarian morphology, a 30% decrease in testosterone levels, and a 25% increase in insulin sensitivity, confirming that TNF-α inhibition reversed the PCOS phenotype.
- Improvement in pregnancy outcomes in clinical studies
STUDY DESIGN: A retrospective analysis that included 100 patients with PCOS showed that the group receiving TNF-α inhibitors (e.g., etanercept) in combination with ovulation induction therapy presented a significant advantage over the control group:
Ovulation promotion efficiency: 1.5 days shorter duration of gonadotropin (Gn) administration and 20% reduction in total dose.
Pregnancy success: clinical pregnancy rate increased to 48.4% (37.9% in the control group), and the rate of high-quality embryos increased to 37.8% (29.0% in the control group).
Safety: 5% reduction in estradiol levels on trigger day and decreased risk of ovarian hyperstimulation syndrome (OHSS).
III. Application strategy and safety of TNF-α inhibitors
- Commonly used drugs and mechanism of action
Etanercept: soluble TNF receptor fusion protein, neutralizes free TNF-α and blocks its binding to cell surface receptors.
Adalimumab (Adalimumab): fully human monoclonal antibody that targets and inhibits TNF-α activity and has a long half-life (~2 weeks).
Infliximab: human-mouse chimeric monoclonal antibody, suitable for moderate to severe cases, requires intravenous administration.
- Necessary premedication screening
Infection risk assessment: need to exclude active tuberculosis, hepatitis B virus carriage, HIV infection and other immunosuppressive risks.
Metabolic index monitoring: including fasting blood glucose, insulin level, lipid profile and assessment of liver and renal function.
- Safety of medication during pregnancy and lactation
FDA pregnancy classification: TNF-α inhibitors belong to Class B. Animal experiments have not shown teratogenicity, and human data show that use during pregnancy does not increase the risk of congenital malformations.
Breastfeeding recommendations: Monoclonal antibody drugs have high molecular weights and very low concentrations in breast milk; interruption of breastfeeding is usually not necessary.
IV. Integrated management: a new paradigm beyond traditional treatment
- Synergy of lifestyle interventions
Anti-inflammatory diet: Increase the intake of omega-3 fatty acids (deep-sea fish, flaxseed), antioxidants (vitamins C and E), and reduce refined sugar and saturated fat.
Exercise prescription: 150 minutes of moderate-intensity aerobic exercise (e.g., brisk walking, swimming) per week, combined with resistance training to enhance muscle insulin sensitivity.
- Gut Flora Regulation
Probiotic supplementation: Lactobacillus and Bifidobacterium can reduce endotoxin (LPS) levels, decrease TNF-α release and improve hyperandrogenemia.
Dietary fiber intake: 25-30 grams of fiber per day (e.g., oats, chia seeds) promotes short-chain fatty acid production and inhibits inflammatory pathway activation.
- Other targeted therapies explored
CMKLR1 receptor antagonist: Preclinical studies have shown that blocking CMKLR1, the receptor for the adipokine Chemerin, ameliorates hyperandrogenism-induced ovarian dysfunction.
Luteolin: a natural flavonoid that reduces estrogen synthesis and alleviates PCOS symptoms by inhibiting aromatase expression.
V. Future prospects: precision medicine and individualized treatment
With the in-depth analysis of the molecular mechanism of PCOS, the traditional “one-size-fits-all” approach will be gradually replaced by precision therapy targeting TNF-α. Combining genetic testing (e.g., TNF-α gene polymorphism analysis) and metabolomic evaluation, individualized drug strategies can be developed to maximize efficacy and minimize side effects. In addition, digital health tools (e.g., AI-driven health management platforms) show potential for patient compliance monitoring and remote intervention, providing a new paradigm for long-term management of PCOS.
相关推荐
- International Reproductive Experts Interpret Successful Strategies and Assisted Reproductive Options in Georgia
- Five Golden Steps to Double Pregnancy Success After IVF Embryo Transfer
- Busting the Three Biggest IVF Lies: International Reproduction Experts Reveal Truths 90% of Families Don’t Know
- Scientific Breakthroughs in 35+ Advanced Fertility Preparation
- Early signs of pregnancy after IVF transfer
Search within the site
Surrogacy News
Hot Tags.
Georgia Surrogacy Services,Legal IVF Hospital,Global Fertility Agency