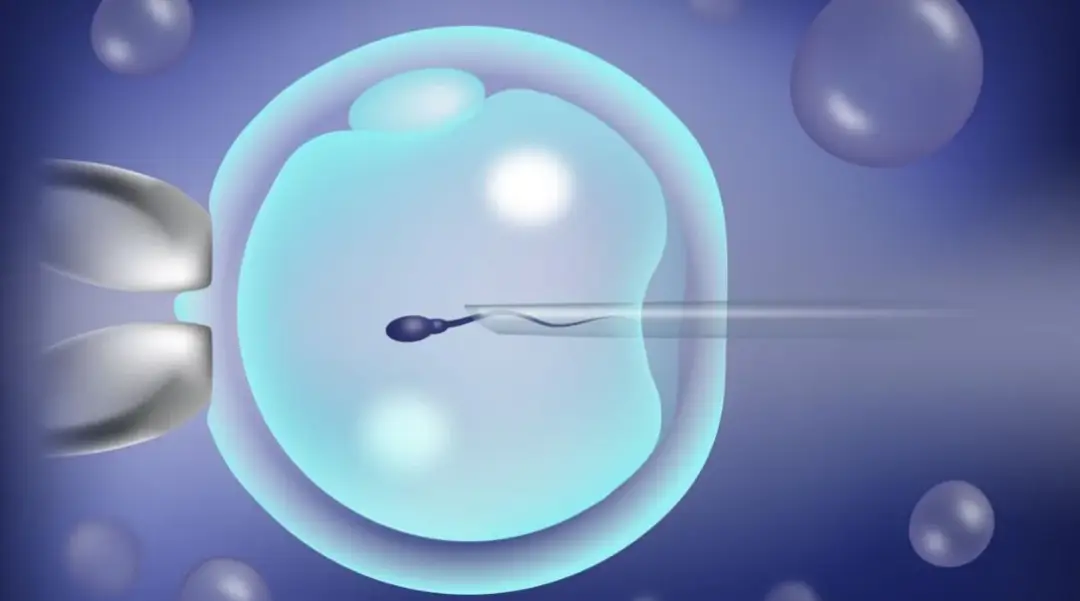
Analysis of the whole process of three-generation IVF technology: a reproductive revolution in the era of precision medicine
Three-generation IVF (PGT, pre-implantation genetic testing) technology has increased the pregnancy success rate to 72% (natural pregnancy rate is about 30%) and the blockage rate of genetic diseases to 99.9%. This article systematically reveals the scientific logic of this life project from four dimensions: technical principle, process innovation, quality control standards and prognosis management.
I. Core principles of PGT technology and screening of indications
- Genetic testing technology matrix
PGT-A (aneuploidy screening): NGS technology detects 23 pairs of chromosomes and reduces the miscarriage rate (from 40% to 15%).
PGT-M (single gene disease detection): SNP chain analysis + mutation locus verification, can diagnose cystic fibrosis, thalassemia and other 7000 + single gene diseases
PGT-SR (structural abnormality screening): whole genome microarray to identify balanced translocations (resolution up to 5Mb)
- Clinical indications stratification
Mandatory indication:
Carriers of chromosomal balanced translocations (spontaneous abortion rate >80%)
Single gene dominant disorders (e.g. Huntington’s chorea, 50% offspring prevalence)
Recommended indications:
≥2 unexplained miscarriages
Repeated implantation failures at advanced age (≥38 years)
Severe male factor (sperm DNA fragmentation rate >30%)
- Technological breakthroughs in genetic testing
Micro-sample processing: single-cell whole genome amplification (MALBAC technology, amplification uniformity >85%)
Artificial Intelligence Interpretation: Deep neural network to recognize embryonic chromosome breakage signals (98.7% accuracy)
Second, the whole process of quality control standards and technological innovation
- Optimization of superovulation protocol
Individualized dosage model:
AMH<1.1ng/ml: microstimulation program (FSH 75-150IU/d) AMH>3.5ng/ml: antagonist regimen (GnRH antagonist 0.25mg/d)
Follicular synchronization technique: biphasic estrogen-progestogen pretreatment (the proportion of follicle diameter difference ≤2mm is increased to 78%)
- Key parameters of embryo laboratory
Dynamic monitoring of incubator:
Oxygen concentration 5% vs 20% (blastocyst formation rate increased by 15%)
EmbryoScope (time-lapse imaging system) records embryo division patterns every 10 minutes.
Sperm optimization technology:
Magnetic Sorting (MACS) to remove apoptotic sperm (40% reduction in DNA fragmentation rate)
PICSI technology to screen hyaluronic acid-bound sperm (fertilization rate increased to 75%)
- Quality control standards for PGT testing
Biopsy window: 5-10 trophoblast cells taken at blastocyst stage (day 5-6)
Assay validation:
Amplification success rate ≥95% (WGA product concentration >1ng/μL)
Chimerism recognition threshold ≥20%
Embryo transfer strategy and pregnancy management
- Endometrial tolerance assessment
ERA testing: transcriptome analysis to determine implantation window (87% accuracy in individualized transfer time)
Three-dimensional ultrasound parameters:
Endometrial thickness ≥7mm
Endometrial blood flow PI <2.5
- Freeze embryo transfer cycle program
Hormone replacement cycle:
Estradiol valerate 6mg/d×14 days
120 hours after progesterone conversion
Natural cycle monitoring: transfer on the 7th day after LH peak (92% synchronization rate)
- Precision management during pregnancy
Early monitoring indicators:
hCG ≥100mIU/ml on day 14 of transplantation (80% live birth rate)
Fetal heart presence rate ≥95% at 6 weeks of gestation
Genetic validation:
Non-invasive DNA testing at 10 weeks of gestation (99.2% compliance rate)
Amniocentesis at 18 weeks of gestation (gold standard for confirming chromosomal abnormalities)
Success rate improvement and risk control
- Factors affecting clinical pregnancy rate
Age and egg quality:
<35 years old: 65% cumulative live birth rate
≥40 years old: cumulative live birth rate decreases to 18
Embryo quality grading:
55% implantation of good quality blastocysts (grade AA)
Grade BC blastocyst implantation rate of 32%
- Complication prevention and control system
OHSS prevention:
Albumin 20g drip after egg retrieval
GnRH agonist instead of hCG trigger
Multiple pregnancy control:
Single embryo transfer policy (twin rate <5%)
Gestational window for fetal reduction: 7-9 weeks (95% survival rate)
- Long-term follow-up data
International Federation for Reproductive Medicine (IFFS) statistics show:
PGT offspring congenital malformation rate 1.3% (natural pregnancy 3%)
No significant difference in neurodevelopmental assessment in childhood
The Future Picture of Reproductive Medicine
Novel technologies are reshaping the field of IVF:
Artificial intelligence embryo rating: convolutional neural network predicts potential (ROC-AUC=0.91)
Mitochondrial replacement technology: oocyte nuclear transplantation to block mitochondrial disease
Ovarian tissue freezing: 83% effective rate of fertility preservation in cancer patients
Three-generation IVF is not only a technological breakthrough, but also a model of individualized medical treatment. Patients are advised to follow the “3-6-9” principle:
3 basic tests (hormone six, semen analysis, hysteroscopy)
6 months of life intervention (BMI control at 18.5-23.9, stop smoking and drinking)
9 key decisions (choice of ovulation promotion program, number of embryo biopsies, transfer strategy, etc.)
The creation of life requires the dual escort of science and technology and humanity, may every expectation meet the dawn of life.
相关推荐
- International Fertility Experts Reveal 4 Golden Rules for Ovarian Function Assessment
- The optimal range for egg retrieval in IVF: 8–15 eggs yield the highest live birth rate
- Why do fertility doctors always advise you to do IVF before it’s too late?
- Scientific Selection Guide for Natural Fertilization vs IVF
- Deadly Warning of Fetal Motion Disappearing at 38 Weeks|International Center for Perinatal Medicine
Search within the site
Surrogacy News
Hot Tags.
Georgia Surrogacy Services,Legal IVF Hospital,Global Fertility Agency